
The Cancer Alliance aims to reduce variation across Humber and North Yorkshire by:
- supporting earlier and faster diagnosis of cancer
- improving equal access to treatment and care
By working collaboratively with partners, we maintain a system-wide overview of cancer services, and support the implementation of interventions to improve performance, including:
- Use of Faecal Immunochemical Tests (FIT) to guide the management of people with symptoms of colorectal cancer
- Introduction of an image pathway for two-week wait and suspected skin referrals
- Achieving Faster Diagnostic Standards across all cancer pathways
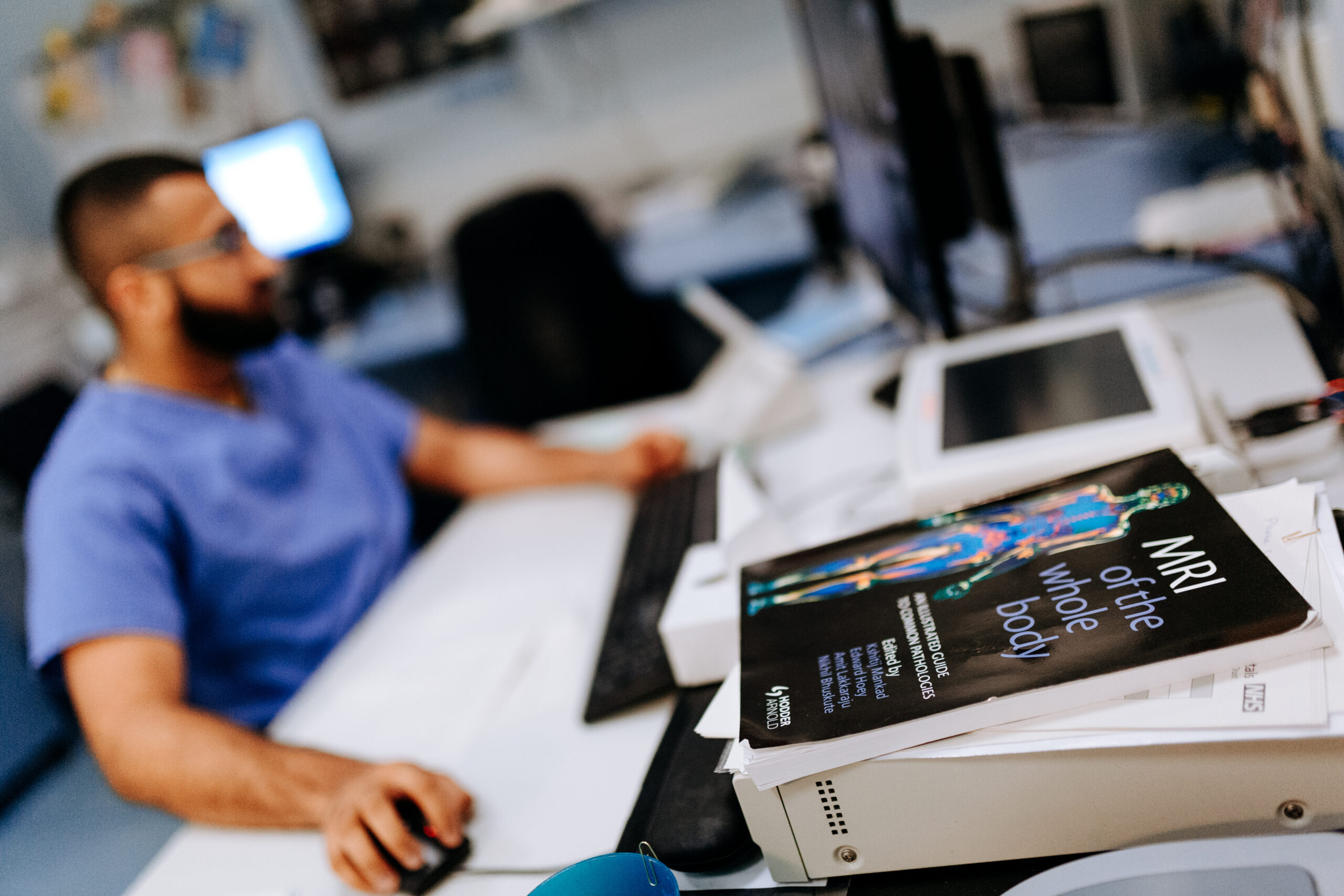
Clinical Delivery Groups
Each of our Clinical Delivery Groups (CDGs) provides an opportunity for clinical leaders to discuss best practice, share challenges, and reduce variation in practice.
CDGs help drive significant changes in the system by uniting people from different:
- Organisations
- Localities
- Programme workstreams
- Neighbouring Cancer Alliances
- Patient and public representative groups
Together, they work collaboratively to develop innovative approaches for the overall wellbeing of the population, especially those impacted by cancer.
More information about Clinical Delivery Groups
CDGs are the source of expert clinical and professional opinion from which advice is sought on a wide range of cancer services issues.
The groups adopt an evidence-based approach, incorporating national best-practice guidance, to ensure an improvement in common standards and pathways. This helps the Cancer Alliance with its vision of ‘achieving world-class cancer outcomes for our communities’.
These are the different CDGs:
- Breast
- Head and Neck
- Gynaecology
- Lower Gastrointestinal - Colorectal
- Lung
- Non-Surgical Oncology
- Skin
- Upper Gastrointestinal
- Urology - Prostate
Faster Diagnostic Standard (FDS)
The Cancer Alliance is supporting the implementation of a new Faster Diagnostic Standard (FDS). The FDS was introduced by NHS England and NHS Improvement to help facilitate a patient-centred flexible and rapid approach to cancer diagnosis/non-diagnosis.
The FDS aims to ensure at least 75% (the national standard) of patients who are referred for the investigation of suspected cancer find out, within 28 days, if they do or do not have a cancer diagnosis.
Clinically endorsed timed pathway guides are being used to implement FDS across all cancer pathways, which has benefits for the groups below.
For patients:
– Empowerment from information about the diagnostic process provided at point of referral
– Reduced anxiety and uncertainty of a possible cancer diagnosis, with less time between referral and hearing the outcome of diagnostic tests
– Improved patient experience from fewer visits to the hospital, particularly with ‘one-stop’ services
– Potential for improved survival by using the faster pathway to prevent patient deterioration
For clinicians:
– Using a nationally agreed and clinically endorsed pathway to support quality improvement and reconfiguration of colorectal cancer diagnostic services
– Working across primary and secondary care to ensure high-quality referrals
– Improved ability to meet increasing demand and ensure the best utilisation of highly skilled workforce
For systems:
– Reduce demand in outpatient clinics (ACE Wave 1 report highlights a 59% reduction in outpatient clinic appointments with implementation of ‘straight to test’ pathway)
– Reduced medically unjustifiable delays in care.
– Improved performance against national standards (particularly 62-day and 28-day standards)
– Improved quality, safety, and effectiveness of care, with reduced variation and improvement in outcome
Image Pathways
We’re working with relevant partners to support the use of images alongside urgent skin cancer referrals across Hull and East Riding of Yorkshire. Image pathways help:
- Support patients
- Manage NHS waiting lists safely
- Cancer services recover from Covid-19.
Skin cancer is one of the most common cancers in Humber and North Yorkshire. We gave 60 new iPhones and dermatoscopes to GP practices. By conjoining the two, healthcare professionals can rule out or diagnose skin cancer earlier, when treatment is often more successful.

Find out more about dermatoscopes
In this video, Dr Dan Roper, Primary Care Lead for Humber and North Yorkshire Health and Care Partnership, explains how dermatoscopes are enabling specially trained GPs to capture and share microscopic images.
Faecal Immunochemical Tests
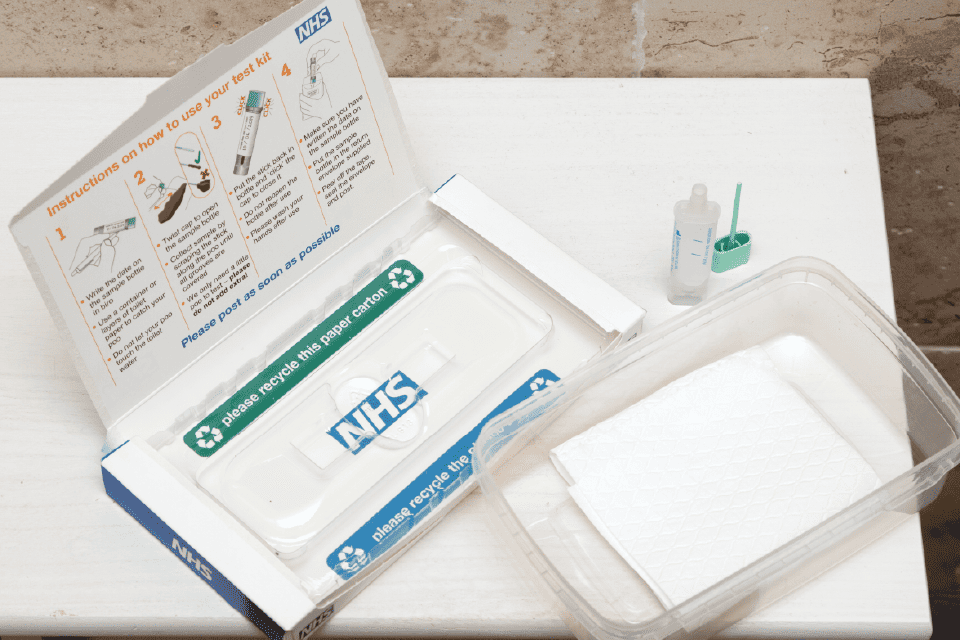
The Faecal Immunochemical Test (FIT) is a type of faecal occult blood test, which detects traces of human blood in stool samples. FIT can be used:
- as the primary test in the NHS Bowel Cancer Screening Programme (BCSP), aimed at individuals without symptoms
- as a test to guide the management of individuals who present with symptoms (symptomatic)
Learn about FIT
Since the start of the coronavirus pandemic, we’ve been working with partners to accelerate the implementation of FIT into the two-week-wait referral process in order to:
- safely manage waiting lists
- improve patient experience
- support faster access to treatment, when required
Find out more about significant differences between each use of FIT here.
