A new initiative to check for liver cancer in high-risk communities has been rolled out as part of a major NHS drive to catch more cancers earlier and save lives.
The roaming trucks performed more than 7,000 fibroscans and identified over 830 people with cirrhosis or advanced fibrosis, a leading cause of liver cancer, in eight months (June 2022 to January 2023) – with the majority of those identified referred on to further care.
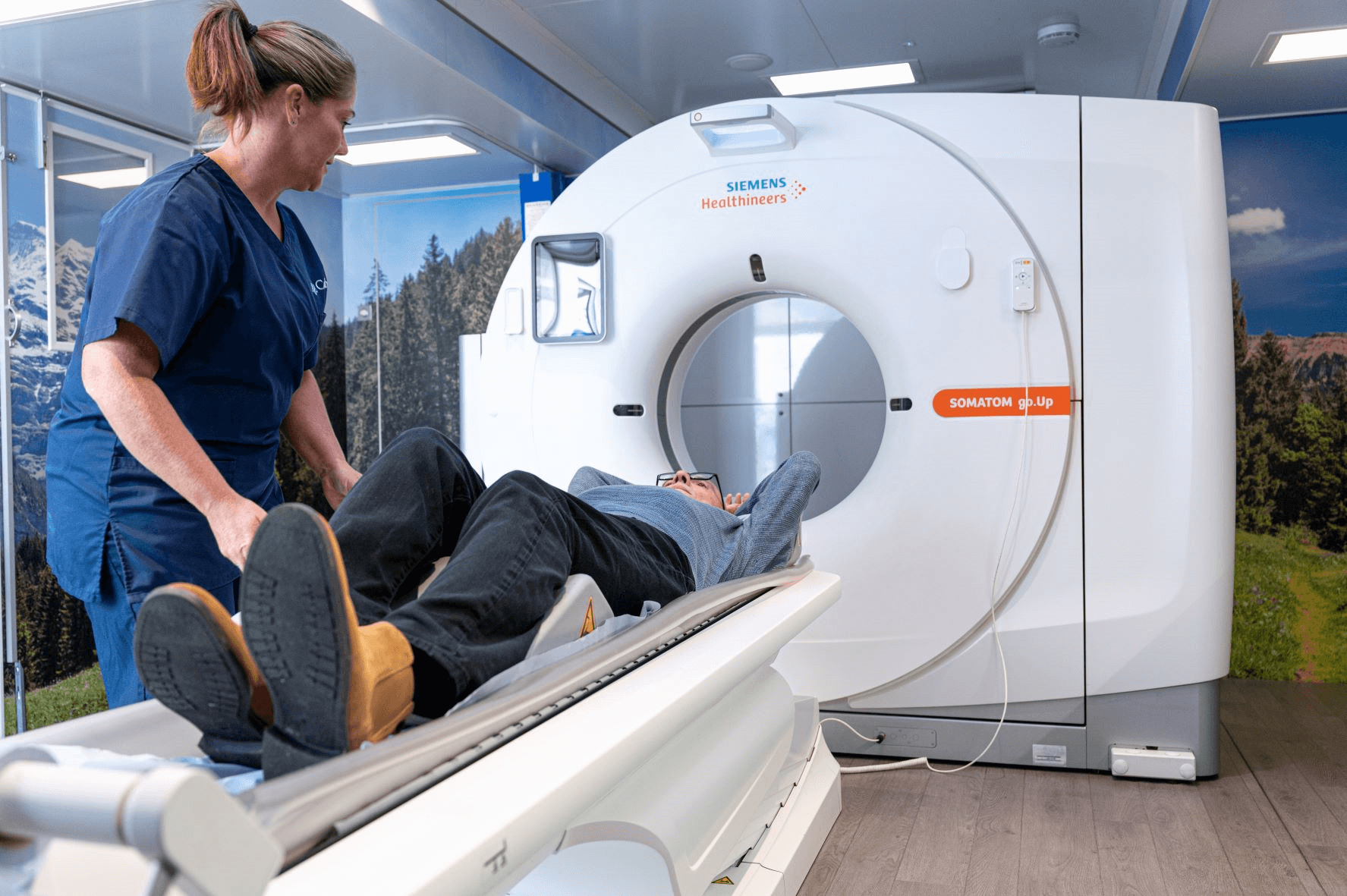
The mobile trucks are visiting high-risk communities across the country at GP practices, recovery services, food banks, diabetes clinics, sexual health clinics and homeless shelters to perform quick, non-invasive scans.
The trucks are expected to visit and scan 22,000 people during the first year of the pilot scheme.
Checks are being offered in the community to adults with high levels of alcohol consumption, a current diagnosis or history of past viral hepatitis, or non-alcoholic liver disease, as these factors increase the risk of developing liver cancer.
NHS staff are already visiting at-risk communities as part of the Hepatitis C Elimination Programme and the programme is being expanded to include a liver health check involving an on-the-spot fibrosis scan which detects liver damage.
Around 6,100 people are diagnosed with liver cancer each year but the number of cases has doubled over the past decade and is expected to continue to rise.
Currently only one in three liver cancers are diagnosed at an early stage, but this programme will help catch more cancers earlier, giving patients a much better chance of surviving the illness. If caught early, patients have a 70-90% chance of survival for five years or more with treatment.
Thanks to the efforts of NHS staff, major public awareness campaigns and targeted screening interventions, more people than ever before are being checked and treated for cancer – with over 2.8 million people checked for cancer and 322,000 starting treatment for cancer in the last year (February 2022 – January 2023).
The NHS has also made significant progress on the 62 day cancer backlog – reducing it by around 10,000 from an all-time high of 33,950 last summer to 22,282 for week ending 26 February 2023, despite record levels of demand on cancer services.
Dame Cally Palmer, National Cancer Director for the NHS in England, said: “Building on the success of other community diagnostic schemes, like our lung trucks, this innovative surveillance programme is bringing lifesaving checks to people who are at a higher risk of liver cancer, and who may have found it difficult to come forward or access health care otherwise.
“The on-the-spot liver scans have already found that around one in ten people in communities visited have advanced liver damage that needs further monitoring or treatment as it could lead to liver cancer – ensuring these people are seen early and referred on for further testing will help us to diagnose cancers at an earlier stage.
“We’ve already seen hundreds of people diagnosed at an earlier stage through our targeted lung cancer trucks, and now with the addition of NHS teams offering these vital liver checks in mobile trucks across the country, I urge anyone who is offered a scan in their community to take up the opportunity.”
Those who are deemed high risk will be provided with information about their level of risk and where appropriate will be referred to their GP. If needed, patients will be referred straight into a six-month liver surveillance care programme, where they will be partnered with a peer support worker who will continue to check in, as well as offer guidance and help informed by people who have experienced liver disease themselves.
The pilot scheme delivers on the NHS Long Term Plan ambition to detect cancer as early as possible so that three in four people have their cancer detected at a very early stage when treatment is more effective. The screening programme means that patients get access to the specialist services they need quickly – regardless of where they live.
Professor Peter Johnson, NHS clinical director for cancer said: “Liver cancer can be hard to detect at an early stage and so these checks, for people who have been identified as higher risk, are an essential part of the NHS’s action to find more people with cancer – and in groups that may otherwise find it hard to access lifesaving tests.
“There are diseases that we know increase the risk of liver cancer, which is why the liver trucks will be visiting particular treatment clinics.
“Lives are saved when cancers are caught early and when more people are referred for tests, which is why the NHS has put so much effort into early diagnosis in recent years, as well as increasing to access to testing.”
Health Minister Helen Whately said: “We know the earlier we detect cancer, the earlier treatment can begin and the better the chance of a patient recovering.
“We are supporting the NHS to bring liver scans into the heart of communities to help tens of thousands of patients to receive a potentially life-saving diagnosis sooner”.
Symptoms of liver cancer include unexpected weight loss, loss of appetite, vomiting blood, and pain or swelling of the abdomen. If anyone has symptoms of liver cancer, they should contact their GP straight away.
The programme will identify those at risk of the most common form of liver cancer, hepatocellular carcinoma (HCC), which makes up 85% of all liver cancers.
Health chiefs have doubled spending on cancer awareness campaigns and continue to encourage people to come forward for checks if invited by the NHS or if they have experienced any worrying symptoms.
Nathan Motherwell, a peer support worker who works for the Hepatitis C Trust in support of the Hepatitis C Elimination programme is visiting communities in Kent to carry out liver checks.
Nathan, who began working for substance misuse programmes in 2007, said he likely had hepatitis C for around 12 years before being diagnosed.
Speaking about the success of the Hep C Elimination Programme, Nathan said: “Thanks to our targeted approach to supporting these at risk communities, we have developed a strong rapport with them which has encouraged more people who otherwise would be reluctant, to come forward for potentially life-saving scans on the community vans.
“Our refer-a-friend scheme has also increased the number of people coming forward for scans and helped identify more people with hepatitis C so that they can get the treatment they need sooner – this shows how impactful a relatable face can be and we hope to replicate this success with the liver check expansion.”
In his peer role, Nathan stays in contact with people who approach the programme, often visiting them to remind them to take medicines and keeping stock of what they have taken.
The work of the Hep C Elimination Programme is also widely known among the wider network of support schemes in Kent, which enables them to refer people to the relevant teams for further help if needed.




 May is Skin Cancer Awareness Month and as the weather across the UK heats up, Humber and North Yorkshire Cancer Alliance has joined forces with Macmillan, SKCIN and MKM Building Supplies to raise awareness of skin cancer and the importance of those working outdoors protecting themselves.
May is Skin Cancer Awareness Month and as the weather across the UK heats up, Humber and North Yorkshire Cancer Alliance has joined forces with Macmillan, SKCIN and MKM Building Supplies to raise awareness of skin cancer and the importance of those working outdoors protecting themselves.