The 2022 under-16 Cancer Patient Experience Survey (U16 CPES) results have been published. Click here to view the results.
The annual national survey, now in its third year, measures children’s cancer and tumour care provided by the NHS in England.
The survey was developed to better understand children and young people’s experience of cancer, which is one of the commitments of the NHS Long Term Plan.
The 2022 survey was completed by 885 patients and parents or carers across England – a response rate of 25%. A response consists of one survey completion for a single patient, which could consist of both parent and child responses.
Children from Humber and North Yorkshire usually receive cancer care at Leeds Teaching Hospitals NHS Foundation Trust or Sheffield Children’s NHS Foundation Trust.
Some of the national findings from the report include:
- 75% of children aged 8-15 reported that they were looked after very well for their cancer or tumour by healthcare staff, compared to 77% in 2021.
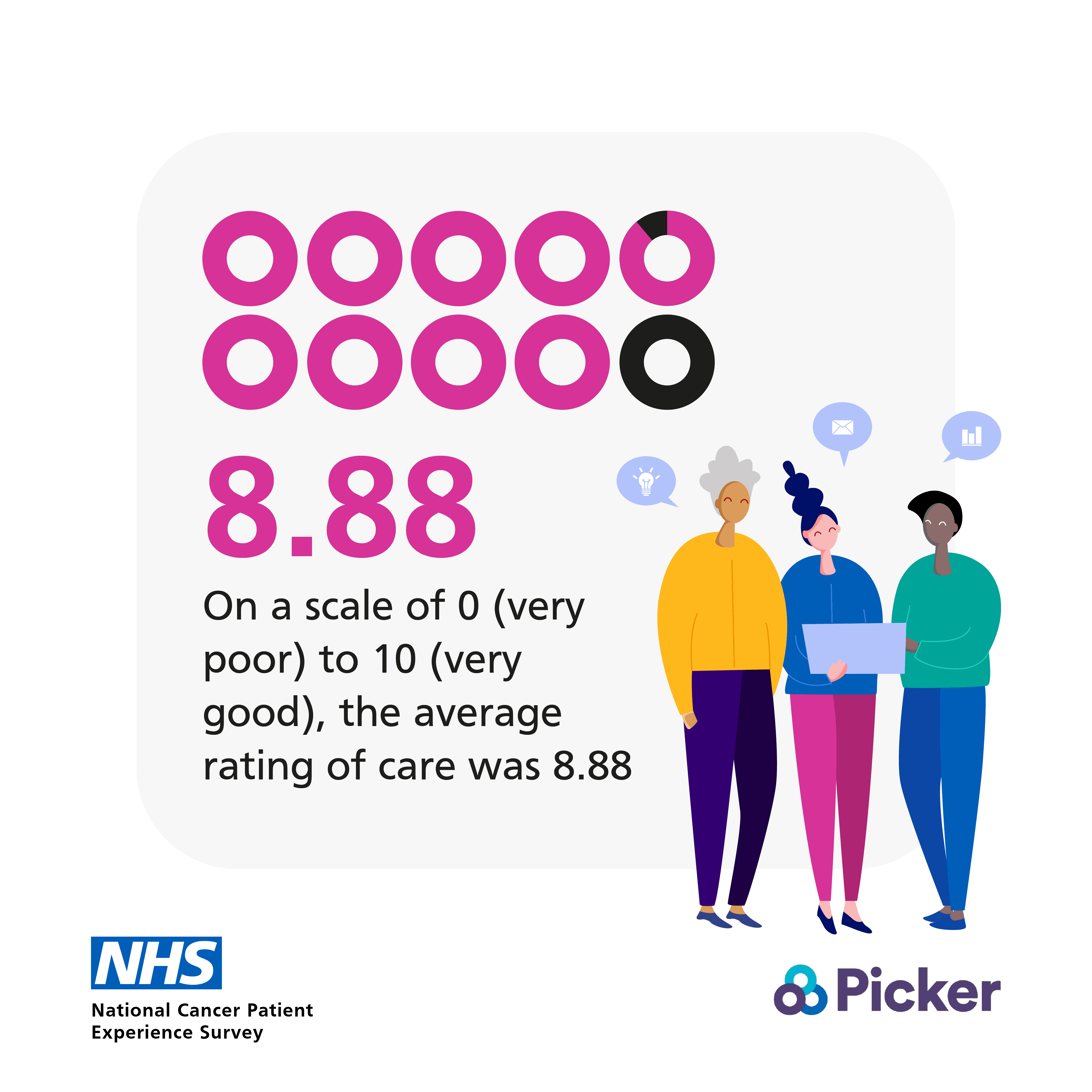
- 89% of parents/carers rated the overall experience of their child’s care as 8 or more (out of 10), compared to 89% in 2021.
- Parents/carers gave a mean rating of 8.99 for the overall experience of their child’s care, compared to 9.01 in 2021.
- Parents/carers of children who were in remission or long term follow up reported a higher score (9.17) than parents/carers of children who were recently diagnosed (8.33), in watch and wait (8.69) and currently receiving treatment (8.89).
- Overall experience scores varied from 8.86 for parents/carers of children living in the least deprived areas in England compared to 9.08 for the parents/carers of children living in the second and third indices of multiple deprivation (IMD) quintiles, 9.03 for parents/carers of children living in the most deprived areas of England, and 9.40 for parents/carers of children living outside of England.
The survey’s respondents are children who were aged between eight and 15 at the point of discharge, and parents or carers of children aged up to 15.
The publication of the under-16 results comes four months after the adult CPES results were published in July.