
Dr Stuart Baugh, Programme Director
Lung Health Checks in Hull
Lung Health Checks in Hull are back following a temporary pause due to the coronavirus pandemic. Thanks to the hard work and dedication of all those involved, we have been able to resume the Targeted Lung Health Check programme and introduce COVID-19 measures to ensure staff and patient safety.
The programme, which aims to diagnose lung cancer early, started its phased return in April and will play a key role in improving outcomes for people at high risk of developing lung cancer or other respiratory diseases.
It has been an incredibly difficult time for cancer services recently and our challenge of diagnosing lung cancer early, when treatment can be simpler and more successful, has only been exacerbated by the coronavirus pandemic.
At the peak of the pandemic, the number of cancer referrals dropped by 60% and although they have recovered well in general, lung cancer has been one of the slowest to recover.
A national ‘Help Us Help You’ campaign which ran between February and May has helped to encourage people with a persistent cough to contact their GP, but there can often be no symptoms during the earliest stage of lung cancer, so it is important to also identify and diagnose those at highest risk of developing the disease.
The Targeted Lung Health Check Programme invites people who are between the ages of 55 to less than 75, are current or previous smokers, live in Hull and are registered with a Hull GP, to take part in a free NHS Lung Health Check.
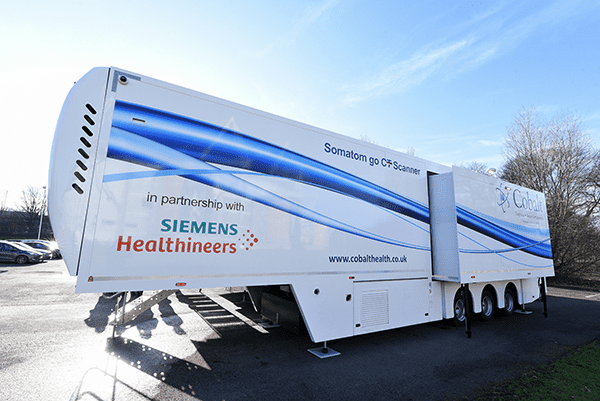
Eligible participants take part in a telephone assessment with a specially trained nurse and those reaching the risk score threshold are then invited to attend a low dose CT scan on board a mobile unit, which is currently situated at Castle Hill Hospital. You can find out more about Lung Health Check appointments in the video below:

We have seen the potential impact of this programme from its initial launch in January 2020. The service ran for five weeks and during that time it welcomed over 900 participants, helped to identify a number of cancers at an early stage and referred over 100 people to local stop smoking services.
As we continue to accelerate Lung Health Checks in Hull, I am incredibly optimistic that we can make a difference to lung cancer outcomes and address some of the health inequalities that exist across our region.
There is a great enthusiasm for this programme both nationally and across the Humber, Coast and Vale area, and as we collaboratively work to roll out NHS Lung Health Checks further, I am looking forward to ensuring more people can benefit from a programme that is at the heart of the NHS Long Term Plan ambitions for cancer.
Dr Stuart Baugh
Programme Director
Targeted Lung Health Checks in Hull

















