The NHS has the opportunity to upgrade cancer screening to save thousands more lives each year, a major report said today.
Leading expert Professor Sir Mike Richards was jointly commissioned by NHS chief executive Simon Stevens and Health and Social Care Secretary Matt Hancock to make recommendations on overhauling national screening programmes, as part of a new NHS drive for earlier diagnosis and improved cancer survival.
In his report, Sir Mike, who was the NHS’ first cancer director as well as the CQC’s chief inspector of hospitals, called for people to be given much greater choice over when and where they are screened.
Women should be able to choose appointments at doctors’ surgeries, health centres or locations close to their work during lunchtime or other breaks rather than having to attend their own GP practice.
Local screening services should put on extra evening and weekend appointments for breast, cervical and other cancer checks.

NHS Targeted Lung Health Checks will take place on a mobile unit.
And as people lead increasingly busy lives, local NHS areas should look at ways that they can provide appointments at locations that are easier to access.
The plan for more convenient checks comes as NHS England is gearing up to roll out lung health checks using scanners on trucks in supermarket carparks and other public spaces.
Sir Mike’s report also called for more to be done to drive uptake through social media campaigns and text reminders. And it called for local initiatives that have successfully boosted uptake to be rolled out nationwide.
In South West London where GP practices have been following up with people who did not attend bowel screening phone calls and reminder letters have led to a 12% increase in attendance. Posting in Facebook community groups has led to a 13% increase in first time attendances for breast screening in Stoke-on-Trent over the past four years.
Sir Mike also recommended a major overhaul to the design of screening programmes.
The NHS is currently upgrading the cervical screening programme with the introduction of ‘primary HPV’ which will reduce the number cervical smears that NHS labs need to review.
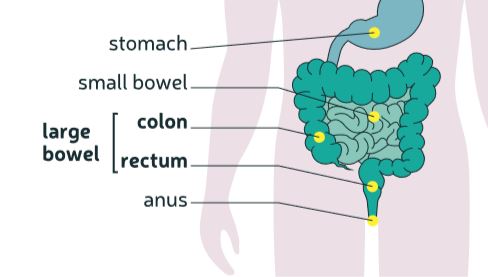
The bowel screening programme is being upgraded by NHS England with a new easier to use ‘FIT’ poo test.
And the £200 million of extra NHS diagnostics investment announced by the Government will upgrade and replace older mammography and diagnostic imaging equipment.
Initial allocations are being made today to NHS providers with equipment that most needs replacing.
These steps all contribute to the NHS Long Term Plan goal of saving an extra 55,000 lives each year within a decade by catching three quarters of all cancers early when they are easier to treat.
Sir Mike welcomed the work NHS England, NHS Digital, Public Health England and NHSX are doing to upgrade ageing IT systems, adding that this process must continue.
This will help screening continue to change over the next decade, and the NHS needs to evolve to adapt to these changes, including the use of artificial intelligence to free up capacity for NHS staff and develop blood tests to screen for a range of cancers.
In future screening will become more personalised, where appropriate using genetics and other factors to determine the risk people face of developing cancer or other diseases and testing them appropriately.
His report also calls for:
- Across all screening programmes, patients should receive results within a standard timetable
- Establishing a single advisory body, bringing together the current functions of the UK National Screening Committee on population screening and NICE on screening for people at elevated risk of serious conditions
- NHS England to become the single body responsible for commissioning and delivery of screening services, ending any existing confusion on who does what
- Breast screening providers should aim to invite people at 34-month intervals after their previous appointment so that all participants can be screened within 36 months
Professor Sir Mike Richards said: “Screening programmes are a vital way for the NHS to save more lives through prevention and earlier diagnosis and currently they save around 10,000 lives every year – that is something to be immensely proud of.
“Yet we know that they are far from realising their full potential – people live increasingly busy lives and we need to make it as easy and convenient as possible for people to attend these important appointments.
“The recommendations in this report are intended to help deliver the commitments set out in the NHS Long Term Plan and will hopefully save even more lives.”
Simon Stevens, NHS chief executive said: “I’m grateful to Sir Mike for taking on this important assignment. His sensible recommendations keep all that is good about NHS screening services, while rightly setting out a blueprint for more convenient access, upgraded technology, and progressively more tailored approaches to early diagnosis.
“He is also right to point to the need to align the expert advice offered to the NHS, and streamline and simplify accountabilities for operational delivery.”
Health Secretary, Matt Hancock said:
“I would like to record my thanks to Professor Richards for his brilliant report, which brings together a substantial number of recommendations.
“After careful consideration, I can announce that Public Health England, our national public health agency, will host world-class scientific and expert advice on screening, building on its current role as host of the UK National Screening Committee. This expert advice will inform the delivery of national screening services by the NHS.”
Click here to view Professor Sir Mike Richards’ report of the Review of Adult Screening Programmes in England.















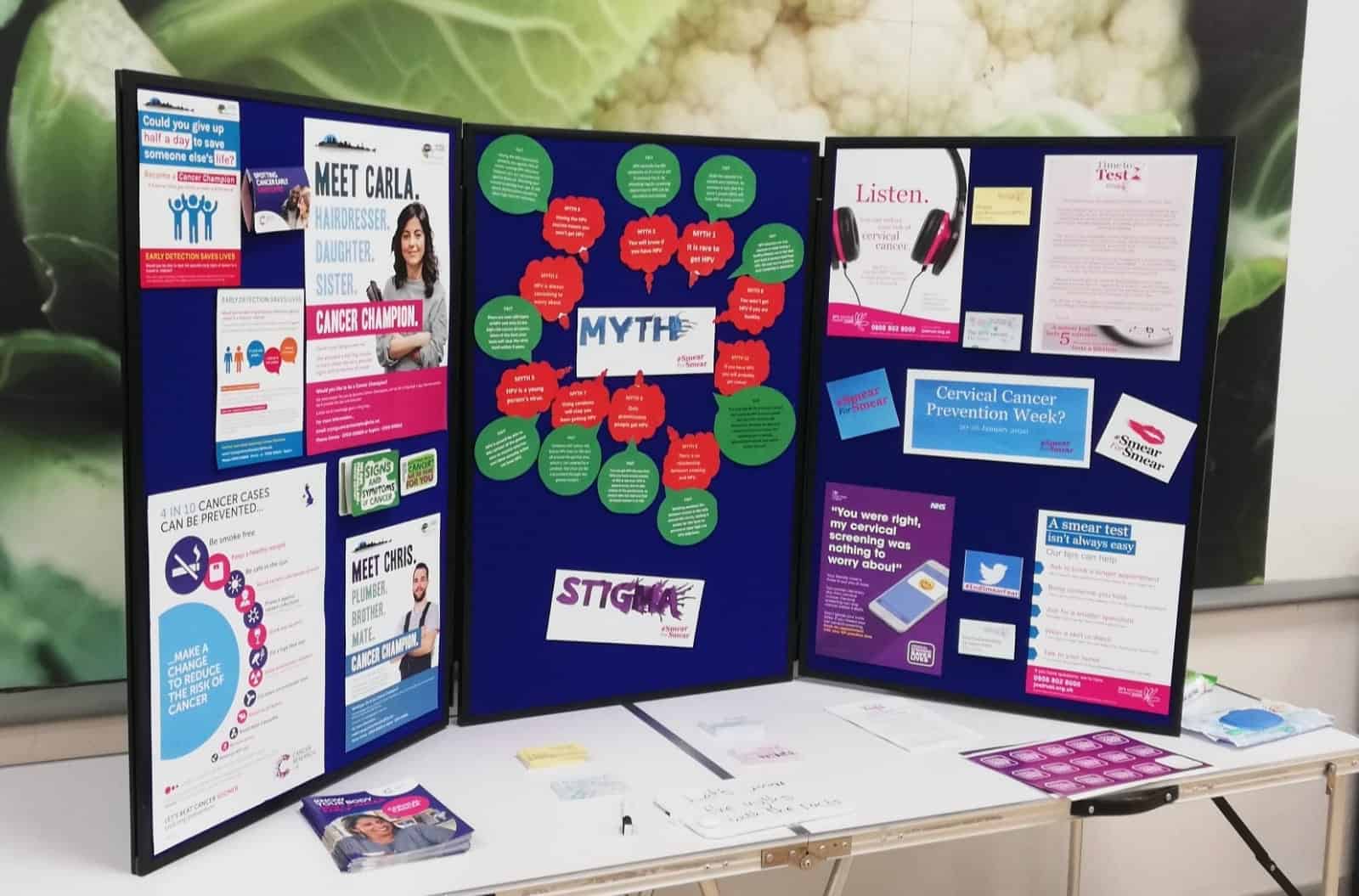 We went out into the community and talked to people about the importance of taking up cervical screening invitations and booking their smear test at their GPs. We also wanted to understand the reason why women didn’t always take up their appointments.
We went out into the community and talked to people about the importance of taking up cervical screening invitations and booking their smear test at their GPs. We also wanted to understand the reason why women didn’t always take up their appointments. We were delighted that three employers across our area signed up to Jo’s Trust’s Time to Test pledge – Vale of York CCG, Unity Health and Photo My Product which encourages employees to attend their cervical screening appointment by giving them time to test.
We were delighted that three employers across our area signed up to Jo’s Trust’s Time to Test pledge – Vale of York CCG, Unity Health and Photo My Product which encourages employees to attend their cervical screening appointment by giving them time to test. 


